The Independent's journalism is supported by our readers. When you purchase through links on our site, we may earn commission.
This psychedelic drug could help treat traumatic brain injuries, new study shows
Hunter Biden is among the most famous former users of ibogaine, derived from the bark of the west African iboga tree
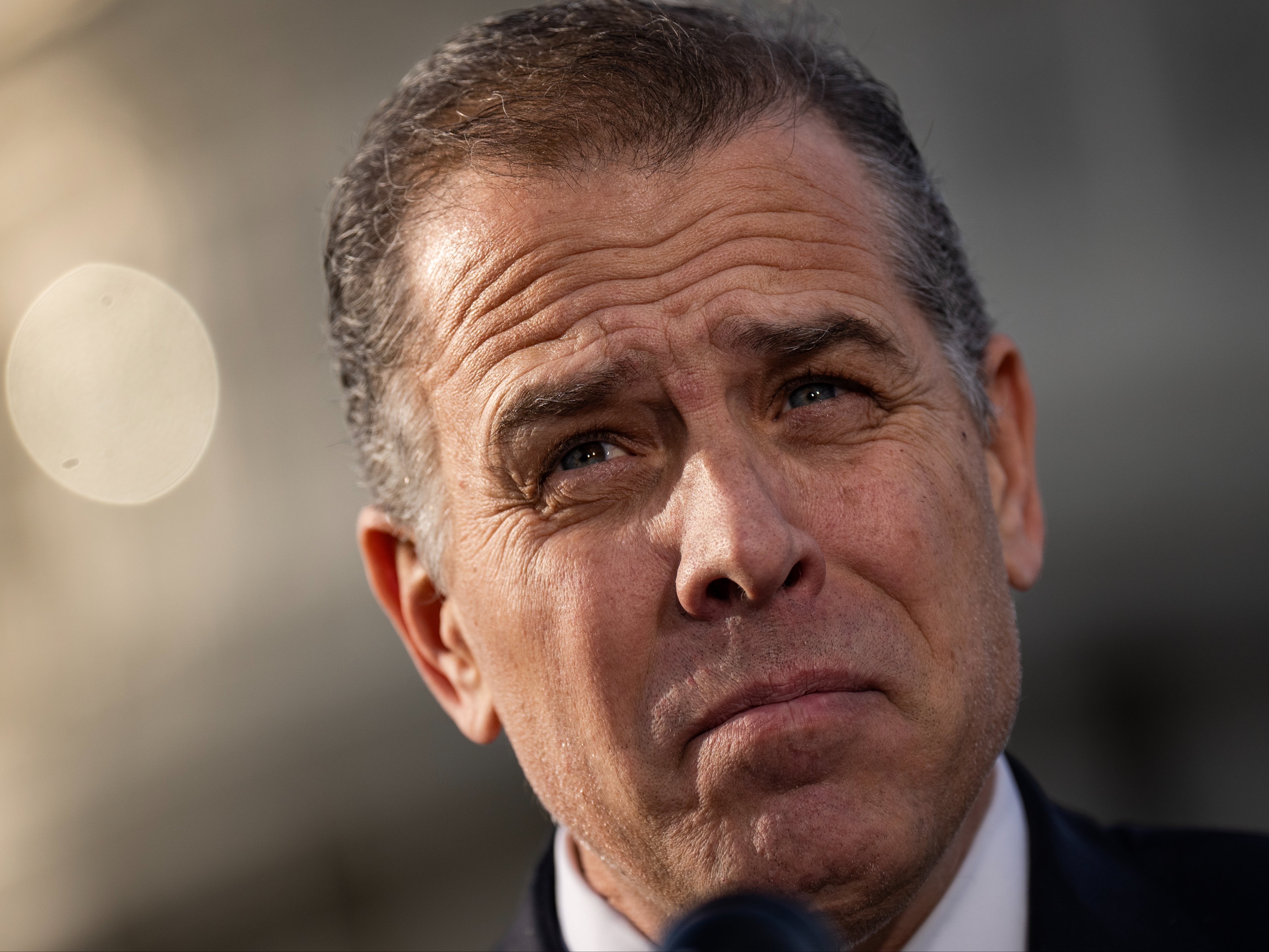
Hunter Biden speaks to reporters outside the US Capitol in December 2023
A west African plant used for centuries in religious rituals may be able to help treat traumatic brain injuries, according to new research.
A study by medical scientists at Stanford University found that ibogaine, a psychedelic drug derived from the bark of the iboga tree, had transformative effects on the symptoms of patients suffering from brain trauma.
The scientists assessed the mental health of 30 US military veterans before and after they travelled to Mexico to be treated with the drug, which has been illegal for both medical and recreational use in the US since 1970.
The veterans' average rating on a scale of disability dropped from 30.2 before the treatment to 19.9 immediately afterwards and only 5.1 one month later, suggesting they would have little impairment in every day life.
However, the range of possible error for those numbers was relatively wide, and the study did not control for the placebo effect, meaning more research will be needed to find out whether the drug is effective and safe.
"No other drug has ever been able to alleviate the functional and neuropsychiatric symptoms of traumatic brain injury," said Dr Nolan Williams, a professor of psychiatry at Stanford and the study's principal investigator.
"The results are dramatic, and we intend to study this compound further."
An increasing body of research over the past few decades has found evidence of medical benefits from psychedelic drugs that are illegal in much of the world, including LSD and psilocybin (found in so-called “magic-mushrooms”).
Ibogaine has long been touted as a potential treatment for addiction, with Joe Biden's son Hunter Biden taking it in 2014 as part of his attempt to stop abusing alcohol and cocaine.
Recently it has also found favour among military veterans afflicted by traumatic brain injuries (TBIs), which occur when the human brain is impaired by some external physical force such as a blow to the head of a nearby explosion and can lead to serious mental health issues such as PTSD.
"These men were incredibly intelligent, high-performing individuals who experienced life-altering functional disability from TBI during their time in combat," Dr Williams said of the study participants.
"They were all willing to try most anything that they thought might help them get their lives back."
Importantly, the study did not include a control group who were secretly given a placebo rather than the real drug, meaning it could not rule out the possibility that these benefits came from some other source than the medicine itself.
The study authors note that it is difficult to create a placebo version of a hallucinogenic drug, because patients generally notice if they are not hallucinating.
Subscribe to Independent Premium to bookmark this article
Want to bookmark your favourite articles and stories to read or reference later? Start your Independent Premium subscription today.

Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies